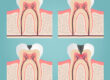
Periodontal disease or more commonly called gum disease, is mainly the result of infection and inflammation of the gum and bone that surround and support the teeth. In its early stage, it’s called gingivitis.
All chronic lifestyle diseases are linked fundamentally by inflammation and pathogenic oral bacteria can be related with several systemic and immune diseases.
A 2020 study published in Neurology suggested that people with severe gum issues were more likely to develop serious cognitive problems.
Ongoing research has shown a possible link between memory loss and oral health. Our mouths contain billions of good and bad bacteria, which release toxins that have the potential to reach the brain.

Additionally, porphyromonas gingivalis, the bacteria associated with unhealthy gums, has been found in the brains of patients with significant memory deficits.
Rheumatoid arthritis, Alzheimer’s disease, pneumonia are just diseases that have been linked to gum disease.
Chronic systemic inflammation caused by a “leaky gut” will affect the mouth. This inflammation could cause oral dysbiosis and “leaky gum”, resulting in periodontal disease and tooth decay.
“Leaky gum” is associated with an increased risk of developing cardiovascular, cardiometabolic and autoimmune diseases.
In effect, if periodontal disease is diagnosed and treated early, it may prevent decades of damage to the brain that result from the toxic effects of oral pathogens.
A change in diet, enhancement of the gut microbiome, the repair of the gut lining, good oral hygiene and modification of some lifestyle choices makes all the difference.
To effectively treat chronic periodontal disease, requires a collaborative care model like a Functional Medicine Model, including a Functional Dentist.